Description, causes, prevention, treatment and medicines
Breast cancer is increasingly common in the Westernised world. As the most common cancer among women it is understandably feared, and discovering a breast lump can be a traumatic experience. Fortunately, most breast lumps are not cancerous. However, for the minority that are, much research has gone into their management. Surgery has moved away from the radical mastectomies of a few decades ago. Breast reconstruction is often on offer. Chemotherapy and hormonal therapy are additional weapons that doctors have at their disposal. So, read on to find out more about breast cancer.
What is breast cancer?
breast cancer
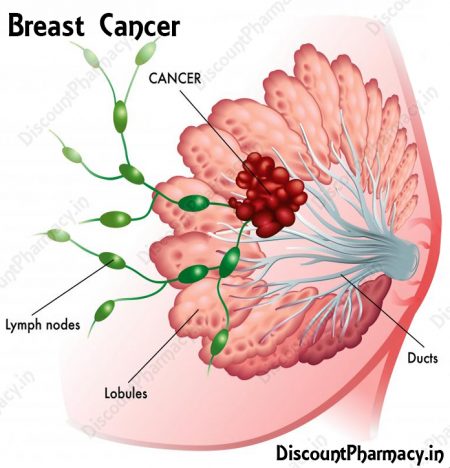
Cancer is a disease where the body’s cells multiply more rapidly than normal. This uncontrolled increase in the number of cells results in a lump which is known as a tumour. These abnormal cells can invade nearby tissues and organs and can also spread through the lymphatic system to other parts of the body. This is why doctors check the lymph nodes under the arm if you have breast cancer — to see if the breast cancer cells have spread to the lymph nodes via the lymphatic system.
Are all breast lumps cancerous?
Not all breast lumps are cancer. In fact most breast lumps are benign — this means non-cancerous.
Fibrocystic changes are a very common cause of benign lumps in the breast. They may make your breasts feel ropy or granular. Fibrosis means the formation of fibrous tissue — this is like scar tissue. More than half of all women will have fibrocystic changes at some stage in their lives, usually before a period begins.
Fluid filled sacs, called cysts, and calcium deposits are other causes of benign breast changes.
A type of benign tumour called a fibroadenoma is a solid, firm rubbery lump which can be moved under the skin when prodded. Fibroadenomas often occur in women during their reproductive years. Benign tumours are not cancer and don’t spread to other parts of the body.
What causes breast cancer?
It is usually not clear what causes the cells to multiply abnormally in breast cancer. The exact cause is unknown. Breast cancer is a complex disease with many interrelated factors and doctors still have much to discover about it.
How would I know if I had breast cancer?
Breast cancer doesn’t usually cause pain in the early stages and there may be no symptoms early on. As the tumour grows, however, symptoms may develop.
Changes that may be noticed with breast cancer are:
- a lump or thickening in the breast or under the arm;
- pitting of the skin over the breast, making it look like orange peel;
- discharge from the nipple — either clear or bloody;
- indenting of the nipple — a pulling back or retracting of the nipple into the breast;
- changes to the size or shape of the breast; and
- warmth or redness or scaly skin on any part of the breast.
If you notice any of these changes or changes like them to your breasts, you should visit your doctor as soon as possible to have them checked out.
Is there a test for breast cancer?
Mammograms — a type of X-ray — are the best way of detecting breast cancer before symptoms develop.
Mammograms are capable of detecting tumours that are too small to be felt. This enables treatment to start sooner than if the tumour was detected when it was larger and able to be felt. The sooner treatment starts the better. In Australia mammograms are recommended for women aged between 50 and 69 every 2 years.
Breast tissue in young women is usually quite dense and mammograms sometimes may not detect lumps. This is why regular mammograms are not usually recommended for women under 40 — along with the fact that breast cancer is rare in younger women.
BreastScreen Australia will perform free screening mammograms to women over 40.
What about breast self-examination?
Some doctors believe that breast self-examinations may not be as useful as previously thought. Some studies have shown that breast self-examination does not lead to fewer deaths from breast cancer and, in fact, may lead to unnecessary biopsies and concern. Cancer associations differ in their positions on whether women should do breast self-exams. One thing is for sure — doing breast awareness/breast self-exams makes you familiar with how your breasts normally feel.
Breast exams should be carried out once a month. If you have gone through the menopause, you should examine your breasts on the same day each month. If you haven’t undergone menopause, the best time is about one week after the start of your last menstrual period.
You should look at your breasts while standing in front of a mirror with your arms up, then with them down by your side, and lastly with them pressed firmly against your hips. Look for lumps, changes in shape or skin dimpling. Next, lie down and systematically feel around your breast in a circling motion as though it were the face of a clock, using your 3 middle fingers. Use your right hand to examine your left breast and vice versDon’t forget to also check under your armpits. You should also examine your breasts and armpits in the shower, using soap and water to help.
Can I inherit breast cancer if it’s in my family?
You may be at increased risk of breast cancer if you have a close family relative who developed breast (or ovarian) cancer. Most women with a family history of breast cancer, however, do not develop it. In fact 8 out of 10 women who get breast cancer do not have a family history of it.
There are inherited defects in several genes that have been shown to put women more at risk of breast cancer. BRCA1 and BRCA2 are 2 of the genes. Women who have inherited specific mutations in either of these genes have a high risk of breast cancer.
What will increase my risk of getting breast cancer?
Many risk factors have been identified that increase the risk of a woman getting breast cancer. Family history is one, which we’ve just discussed and it can’t be changed.
Here are some other risk factors that you can’t influence.
Age — as you get older your risk of developing breast cancer increases. Breast cancer is rare in women under 35.
Having already had breast cancer.
Having a defect in the BRCA1 or BRCA2 gene — as discussed, having a defect in these genes increases your risk.
Menopause — if you have a late menopause (after 55), you are exposed to oestrogen for longer than other women and have an increased risk of breast cancer.
Menarche — if your first period came before age 12, you are exposed to oestrogen for longer than other women and have an increased risk of breast cancer.
Women whose mothers took the medicine DES (diethylstilboestrol, a synthetic oestrogen that was used to prevent miscarriage from the 1940s through to 1971) during pregnancy have an increased risk of breast cancer. (The mothers who took DES have a much smaller increased risk of breast cancer.)
Having been previously diagnosed with a non-invasive breast condition such as ductal carcinoma in situ (DCIS) or lobular carcinoma in situ (LCIS) increases your breast cancer risk.
Are there risk factors that I may be able to influence?
Yes, here are some risk factors that you may be able to influence.
Excess weight — putting on excess weight as an adult, especially after menopause, increases your risk of breast cancer.
Alcohol consumption — having more than 2 standard drinks of alcohol per day is associated with an increased risk of breast cancer, and the risk is further increased with each additional standard drink per day.
Taking combination (oestrogen and progestogen) hormone replacement therapy for 5 years or more has been shown to increase the risk of developing breast cancer.
Taking the oral contraceptive pill slightly increases your risk, although the risk levels return to normal within 10 years of stopping the pill.
Is there anything that can reduce my risk of breast cancer?
There are some things that are thought to be protective against breast cancer, including:
- getting regular physical activity (studies have shown that brisk walking for 1.5 to 4 hours per week reduces breast cancer risk in postmenopausal women);
- having children (the more children women have, the more their risk appears to be reduced);
- having children before the age of 30; and
- breast feeding for a total of 12 months or longer.
Will taking hormone replacement therapy (HRT) increase my risk of breast cancer?
Results of a large US trial published in 2002 showed an increased risk of developing breast cancer with long-term HRT use. The Women’s Health Initiative trial into the use of combined HRT (containing oestrogen and progestogen) was stopped after 5 years because women treated with the HRT combination had a higher risk of invasive breast cancer than women treated with dummy tablets. This would equate to 8 more invasive breast cancers per year for every 10,000 women treated. Since this trial was published, the rate of HRT use dropped and there has been a corresponding decline in the rate of breast cancer.
Women who have been taking a combined formulation of HRT (oestrogen plus progestogen) should review their treatment with their doctor if they have not already done so. Combined HRT can still be used as a short-term treatment for severe menopausal symptoms, for instance to relieve hot flushes, but treatment needs to be reviewed with your doctor regularly — at least every 6 months.
Are there different types of breast cancer?
Yes. The most common type of breast cancer starts in the ducts and is called ductal carcinomLobular carcinoma starts in the lobules of the breast. The lobules are the small sections of the lobes that end in lots of tiny bulbs where breast milk is produced.
Some breast cancers can be stimulated to grow by hormones, such as oestrogen and progesterone. These cancers are known as oestrogen receptor-positive and progesterone receptor-positive, because they have oestrogen and/or progesterone receptors on the surface of the tumour cells. A tumour that is hormone receptor-positive may respond to hormone-blocking medicines, such as tamoxifen.
How is breast cancer diagnosed?
When you go to your doctor after finding a change in your breast, the next step is usually that the doctor examines the breast and then will send you for a mammogram. If the mammogram raises suspicion, your doctor will probably suggest a fine needle biopsy to take a tiny sample of the cells from the lump. A more substantial biopsy may be taken if necessary. Sometimes ultrasound is used to distinguish between a solid lump and a cyst, which is filled with fluid. Ultrasound is also used in younger women whose breast tissue is usually quite dense — and where it is often difficult to detect lumps on a mammogram.
If a biopsy finds cancer cells, then more tests are carried out to find out the characteristics of the cancer cells. For example, do they have oestrogen receptors? These are known as oestrogen receptor-positive. These tumours grow more slowly than other tumours and can often be treated with hormone-blocking drugs, such as tamoxifen.
Are the cancer cells of the type that will spread quickly or not? A pathologist will examine the cells taken from a biopsy to get a picture of the cancer cells and how they might behave.
How will I know if the cancer has spread?
If breast cancer is diagnosed, your doctor may order blood tests, bone scans or X-rays to see if the cancer has spread to other parts of the body, particularly if it appears advanced. But, at the moment, there is no reliable method of telling for sure whether the cancer has spread to other parts of the body away from the breast, as some of these secondary sites may be microscopic. The best forecast of future recovery is whether and to what degree the cancer has spread to the lymph nodes in the armpit.
What is sentinel node biopsy?
Lymphatic fluid bathes the tissues of our bodies and then drains via the lymphatic system of vessels to lymph nodes where the lymph is filtered of cancer cells and bacteria etc. The lymphatic system of vessels is a network covering the body, much like the blood vessels of the circulatory system.
A sentinel node is the first lymph node to receive the drainage from a tumour and therefore would be the first lymph node to develop cancer.
Sentinel node biopsy is a technique whereby a surgeon injects blue dye or a radioactive tracer into the breast near the tumour. As the dye or tracer drains away into the lymph nodes in the armpit, the surgeon can see the first lymph node that the dye reaches. This is the sentinel node. The surgeon removes the node, examines it and sends it for testing to see if it contains cancer.
The assumption made is that the sentinel node is a good indicator of the status of the other lymph nodes that the tumour drains to. If the sentinel node contains cancer, it is removed, along with its surrounding nodes and any other suspicious nodes. But if the sentinel node is clear, removal of the lymph nodes may be unnecessary and so the risk of surgical side effects, such as lymphoedema, are avoided.
What are the treatments for breast cancer?
If a diagnosis of breast cancer is made, your doctors will tell you the options you have for treatment, based on the type of cancer you have and how far it has spread.
Breast cancer treatment options include surgery — breast conserving surgery and mastectomy — radiation treatment, chemotherapy and hormone-blocking medications. Sometimes a combination of treatments is needed. If the tumour is confined to the breast, surgery is usually carried out.
What are the different types of surgery?
Surgery will either be to remove the whole breast (this is called mastectomy) or the tumour and some of the normal tissue surrounding the tumour (this is called breast-conserving surgery). One type of breast-conserving surgery is lumpectomy, where the cancer is removed along with a margin of normal tissue from around it.
Surgery also usually involves removal of some of the lymph nodes from under the arm.
The most common treatment for early breast cancer is breast-conserving surgery with removal of the lymph nodes followed by radiotherapy.
Are there any side effects from surgery?
Unfortunately, lymphoedema is sometimes a byproduct of breast cancer surgery. Lymphoedema is an obstruction of the normal drainage of lymphatic fluid (lymph) from body tissues, which causes swelling (oedema). Breast cancer surgery that involves removal of some or all of the lymph nodes in the armpit can sometimes lead to lymphoedema — swelling of the arm. This is because the lymphatic fluid can’t be drained from the arm and builds up. Lymphoedema may affect one in 5 women after breast cancer surgery and also can occur after radiotherapy.
Will I be able to have a breast reconstruction?
Many women who have a mastectomy choose to have a breast reconstruction carried out. It can be done at the same time as the mastectomy or later. There are a few methods of breast reconstruction and your doctors and surgeons will be able to advise which are suitable for you. Not all methods will be suitable for everyone.
What about radiotherapy?
Radiotherapy uses high-energy X-rays to kill cancer cells and shrink tumours. It is usually carried out a couple of weeks after surgery. A usual course of radiotherapy for breast cancer would involve treatment 5 days a week for between 3 and 7 weeks.
The radiologist may need to mark your skin so that the radiation is directed to the correct areThe radiation doesn’t hurt and you shouldn’t feel any discomfort.
Radiotherapy does not make your hair fall out, but near the end of your treatment period you may feel tired and your skin may take on a sunburned look where it has been treated.
Are there medicines to treat breast cancer?
Nowadays, most breast cancer patients are offered treatment with hormone therapy or chemotherapy if these are appropriate.
Hormone therapy, such as tamoxifen (e.g. Nolvadex) or toremifene (brand name Fareston), is only appropriate if your tumour is oestrogen receptor-positive and/or progesterone receptor-positive — that is, it has oestrogen and/or progesterone receptors on the cells. Hormone therapy blocks the oestrogen that encourages the tumour cells to grow. (About 5 per cent of women with breast cancer have progesterone receptor-positive, oestrogen receptor-negative cancers. Despite lacking oestrogen receptors, some of these women may benefit from hormone therapy – you should discuss the possible benefits with your doctor.)
Other, newer medications called aromatase inhibitors are also used in hormone-dependent breast cancers. These include anastrozole (brand name Arimidex) and letrozole (brand name Femara).
Other ways to reduce the amount of oestrogen feeding an oestrogen receptor-positive tumour are: surgery to remove the ovaries; radiation of the ovaries; and a hormone implant called goserelin (brand name Zoladex) which is used in women who haven’t gone through the menopause yet.
About 20 per cent of breast cancers are HER2 positive. This means that the breast cancer cells have high levels of a protein called human epidermal growth factor receptor 2 (HER2) on their surface. The HER2 protein stimulates the growth of new cancer cells, and high levels can be associated with a poorer outlook. Women with HER2 positive breast cancer may benefit from treatment with a medicine called trastuzumab (brand name Herceptin) in addition to standard therapy. Herceptin targets the HER2 protein, attaching to the HER2-positive cancer cells and stopping them from growing and dividing.
What is chemotherapy?
Chemotherapy may use a combination of any of about 50 drugs to kill cancer cells. They can be given by injection, by pills or by injection into a vein (intravenously), depending on the drug. CMF is a common combination of 3 drugs (cyclophosphamide, methotrexate and fluorouracil) which has been used for many years now. The anthracycline drugs, such as doxorubicin (e.g. Adriamycin) or epirubicin (Pharmorubicin), are other drugs used in chemotherapy. Still more medicines used in chemotherapy for breast cancer are the drugs called taxanes. These include paclitaxel (e.g. Taxol) and docetaxel (Taxotere).
Chemotherapy does have side effects, such as temporary hair loss, nausea and vomiting and tiredness. You may be given medicines to help with the nausea and vomiting.
What chance is there that my breast cancer will come back?
It is very difficult to quantify the risk for an individual, as so many factors come into play. Although it’s true that breast cancer can return later on, most relapses happen in the first 5 years after diagnosis. The later the relapse happens, the more likely it seems to be that the person will respond to further treatment.
In terms of outlook, what is known is that the less involved the lymph nodes are, the better the chance of surviving. If no cancer is found in the lymph nodes or cancer is found in one to 3 nodes this gives a better chance of surviving 10 years than if cancer is found in, say, 10 lymph nodes.
Another indicator of outlook is how the cells look under the microscope. Doctors and pathologists can often tell how aggressive a cancer is by looking at the shape and form of its cells.
Surprisingly, some women who have survived a breast cancer diagnosis say that it has had some positives as well as the expected negatives. They say it made them focus on what’s important to them and to their families. Surviving breast cancer made them stronger and made their relationships deeper and more enriched.